What is Ketamine?
Ketamine is often thought of as a horse tranquilizer because it is highly effective at sedating animals with intramuscular injections. In human medicine, we usually administer ketamine intravenously (IV) because it allows for more precise control over the dosage, especially important during surgery or in emergency room settings. Ketamine has been safely used in humans for over 50 years.
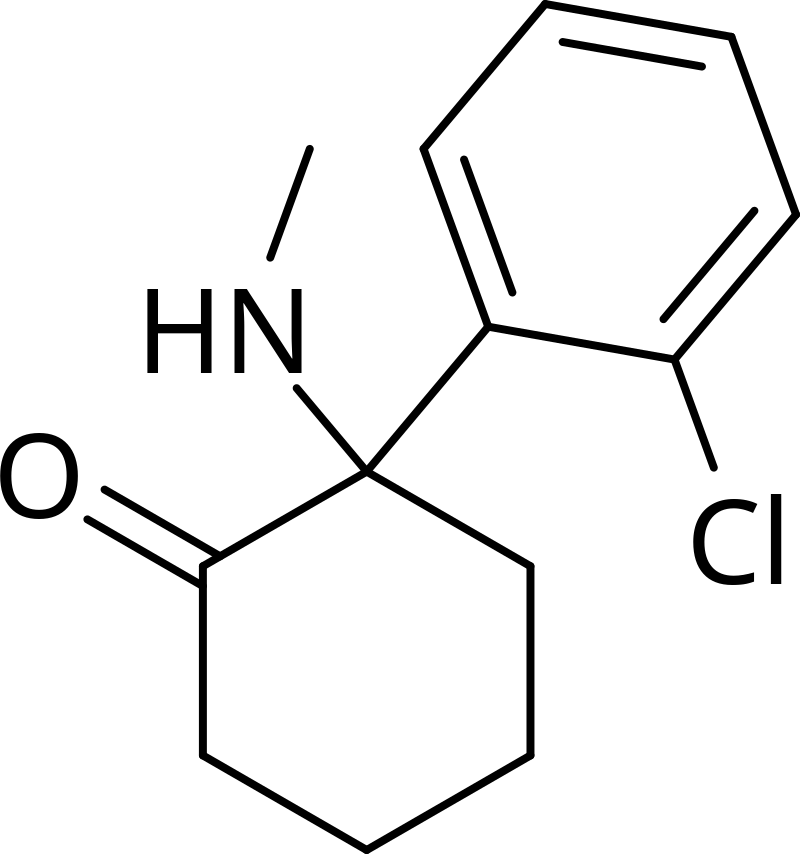
Ketamine is an anesthetic used in the operating room and emergency room due to its unique properties, such as allowing patients to breathe even at relatively high doses. This makes it ideal for sedation without the need for a breathing tube. Ketamine primarily acts at the NMDA receptor, affecting the neurotransmitter glutamate. However, it also interacts with many other receptors in the brain, and its exact mechanism of action remains not fully understood.
How Does Ketamine Work?
The effects of ketamine are dose-dependent:
- High Doses: Can induce complete anesthesia, rendering the patient unconscious and potentially affecting breathing.
- Moderate Doses: Useful for pain control without fully sedating the patient.
- Low Doses: Induce a dissociative state, allowing individuals to enter a highly healing mental space.
At low doses, ketamine can help patients with cognitive rigidity—being stuck in a particular mindset, often seen in mental health conditions like depression, anxiety, PTSD, and chronic pain. Ketamine induces neuroplasticity, helping to rewire the brain and soften rigid thought patterns, leading to persistent changes in self-representation and perspective.
Forms of Ketamine Administration
Ketamine can be administered in various forms:
- Intramuscular (IM): Used in veterinary settings and emergencies where IV access is not feasible.
- Oral: As lozenges or pills.
- Intranasal: As a spray.
- Intravenous (IV): The gold standard for fast and controlled administration, especially useful in clinical settings for quick onset of action.
Effects and Benefits of Ketamine
Ketamine helps patients revisit themselves and enter a psychedelic state at low doses, which can be very therapeutic for mental health conditions characterized by rigid thought patterns and cognitive distortions. Patients often report feeling lighter, more optimistic, and connected to the world around them after ketamine therapy. It helps transition from inward-focused rumination (depression) or future-focused anxiety to a broader perspective, embracing connections with people, nature, and the world.
Risks of Ketamine
While ketamine has many therapeutic benefits, it also carries risks:
- Addiction: Ketamine is a scheduled drug with potential for abuse, requiring careful dosing and supervision by trained professionals.
- Bad Trips: The most significant risk in a clinical setting is a bad experience or “k-hole,” where a person becomes overly dissociated. This can be frightening and counterproductive, potentially deterring patients from future beneficial psychedelic experiences.
To minimize risks, it’s crucial to have ketamine administered by board-certified, trained professionals who can guide patients safely through their experience.