Bulimia Nervosa, commonly known as bulimia, is an eating disorder characterized by repeated episodes of binge eating followed by compensatory behaviors to prevent weight gain. While it shares similarities with anorexia nervosa, bulimia typically involves individuals maintaining a normal or elevated weight, whereas anorexia involves an intense fear of gaining weight and behaviors that lead to significant underweight.
Prevalence and Demographics
Bulimia is most commonly seen in females, approximately three times more often than in males, with the peak age around 20 years. While less common in children, the incidence appears to be increasing. The lifetime prevalence by age 20 in females is about 2.6%, and between ages 13 and 18, it is roughly 1%. Factors associated with the development of bulimia include early puberty, history of sexual abuse, media pressure, childhood obesity, and a family history of substance abuse or eating disorders.
Signs and Symptoms
Individuals with bulimia often feel ashamed and may not openly discuss their eating behaviors. Key symptoms include:
- Binge Eating Episodes: Consuming an excessive amount of food in a discrete period (e.g., two hours) with a sense of loss of control.
- Compensatory Behaviors: Efforts to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, enemas, fasting, and excessive exercise.
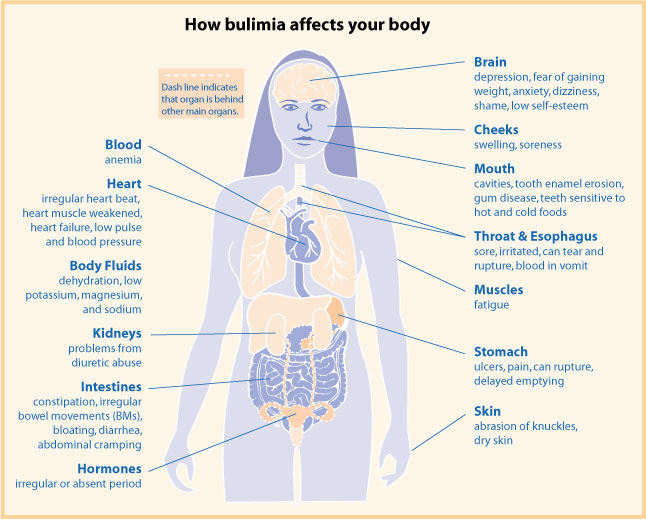
Physical Indicators
- Russell’s Sign: Calluses on the dorsum of the hands from inducing vomiting.
- Dental Erosion: Caused by stomach acid from repeated vomiting.
- Parotid Gland Hypertrophy: Swelling of the glands due to repeated stimulation of taste receptors from vomiting, reported in nearly 70% of cases.
Associated Psychological Features
Common psychological traits include dissatisfaction with body image, perfectionism, and histories of anxiety, depression, or obsessive-compulsive disorder (OCD). Menstrual irregularities are also frequent.
Complications
- Cardiac Arrhythmias: Often due to hypokalemia or hypomagnesemia, potentially manifesting as palpitations or syncope.
- Suicide Risk: Should be considered during evaluation.
- Esophageal Rupture: Conditions like Mallory-Weiss tear or Boerhaave syndrome due to repeated vomiting, presenting with hematemesis.
Diagnosis
Diagnosis is based on the DSM-5 criteria, which require:
- Binge Eating Episodes: Including a sense of lack of control.
- Recurrent Compensatory Behaviors: To prevent weight gain.
- Frequency: Both behaviors occur at least once a week for three months.
- Self-Evaluation: Unduly influenced by body shape and weight.
- Exclusion: Behaviors do not occur exclusively during episodes of anorexia nervosa.
Laboratory investigations may be conducted to assess for complications such as electrolyte imbalances and anemia.
Treatment
Cognitive Behavioral Therapy (CBT): The first-line treatment, particularly using a guided self-help approach, aims to:
- Increase motivation for change.
- Replace dysfunctional eating patterns with regular and flexible ones.
- Decrease undue concern with body shape and weight.
- Prevent relapse.
CBT is estimated to eliminate binge eating and purging in 30 to 50% of cases.
Interpersonal Psychotherapy: Another option with evidence supporting its effectiveness in reducing binge eating episodes.
Pharmacological Therapy: Often used as an adjunct to psychological therapies, including:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Fluoxetine is approved for treating bulimia in adults and for OCD and depression in pediatric populations.
- Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs): Used alongside psychological therapy to address comorbid psychiatric conditions like OCD or major depressive disorder.